Cancer | 10 min read
Here's What You Should Know About Testicular Cancer
Medically reviewed by
Table of Content
Synopsis
The cancer of the male reproductory organ, the testis or the testicle, is termed testicular cancer. Testicular cancer is the most common cancer affecting males between the ages of 15 and 45. The mode of treatment and the body's reaction to it depends on the cancer-cell type, the extent of metastasis, and the patient's overall health.
Key Takeaways
- Testicular cancer is the cancer of the male testis, and it can be detected by self-examination
- A family history of testicular cancer or undescended testes increases the chances of developing the disease
- It is a curable form of cancer that can be eradicated using surgery, radiation, and chemotherapy
What is Testicular Cancer?
The cancer of the testis, or the testicle meaning the male reproductive organ, is termed testicular cancer. The testis (plural testes) rests within a loose sack of skin called the scrotum, placed beneath the penis. The primary function of the testes is to produce sperm and male hormones (androgen), especially testosterone. It is thus a crucial part of the male reproductive system, and its health needs to be kept in check over time.
Males between the age range of 15 and 45 are most prone to this type of cancer. However, if diagnosed at an early stage, it can be treated and cured with much ease and efficiency, averting the risk of death.
The mode of treatment and the body's reaction to it depends on the cancer-cell type, the extent of metastasis, and the patient's overall health. The first step in the detection is to conduct a testicular cancer test which involves testing for tumour cell markers.
This type of cancer can be detected by oneself through a self-examination. It is thus crucial to be aware of how a normal testis looks and feels and immediately do an oncologist consultation if anything about it feels out of the ordinary.
Testicular Cancer Causes
A handful of factors lead to the causation of testicular cancer. The basis of the origin of cancer is uncontrolled growth in the cells of the testis due to mutations or external factors. Some of the testicular cancer causes are listed below. Genetics:
Possessing a family history of testicular cancer increases the chance of developing it. If a male individual's father, brother, or close relative has suffered from the disease, he is more prone to it. It is advisable for such individuals to conduct a self-exam every alternate month to keep track of their testes. Studies showed having a brother with a history of the disease increased the risk from 8 to 10-fold while having a father with exposure increased it to 4 to 6-fold [1]. Research has concluded that one of the major risk factors for this type of cancer is the E2F1 gene copy number variations [2].
Undescended testes (cryptorchidism)
Certain boys are born with their testes inside their abdomen, but after the first year, they naturally descend into the scrotum. However, if they fail to descend, they should be surgically moved via what is called an orchidopexy to position the testes where they rightfully belong. If the testes remain undescended, there is a significant chance of developing cancer as opposed to those having their testes within their scrotum.
According to a few studies, cryptorchidism has indicated a 3.7–7.5 times higher predisposition to testicular cancer than those having scrotal testes [3].
History of cancer
If someone has already had testicular cancer in one testis, it is likely that he will develop the same in the other testis. Therefore, frequent check-ups and self-exams should be ensured in order to prevent that.
Race
People belonging to countries like Europe and the United States are more prone to testicular cancer than other countries.
Early Signs and Symptoms of Testicular Cancer
Testicular cancer symptoms generally get reflected in one of the two testicles. If any of the following symptoms are encountered, it could be a sign of testicular cancer.
- Detection of a lump, typically painless, within the testis- If caught early on, the lump may be the size of a marble, but with the progress of time, it can grow in size
- Any pain or sense of discomfort in the testicle
- Swelling in the scrotum
- Feeling of tenderness in the male breast tissue- Due to hormonal imbalance, there might be swelling of the breast tissue, a condition known as gynecomastia
- A slight sensation of pain in the lower belly or groin
- Fluid build-up in the scrotum
Upon detection of any of the above symptoms via self-examination, it is imperative to visit a doctor to confirm the condition. It is plausible that the symptoms could also be reflective of other ailments, including hernia, epididymitis, hydrocele, or even testicular torsion.
Testicular Cancer Types
The testicles constitute different types of cells, and each cell type gives rise to another type of testicular cancer. Germ cells are the most common type of cell that gives rise to this cancer. The type of testicular cancers that emerge from germ cells are
Seminomas
These are slow-growing cancers that raise HCG levels. The best means of treating seminomas is through radiation and chemotherapy. There are two categories of seminomas; classical and Spermatocytic. The latter is less likely to metastasize as compared to the former.
Non-seminomas
These are more rapidly growing cancers and are less responsive to radiation as well chemotherapy. Typically, surgery is used to treat this type of cancer. Non-seminomas are of four types:
- Yolk sac carcinoma looks like the yolk sac of an early human embryo. If they occur in adults, it is of serious concern in terms of treatment. Generally, if detected in children, it can be eliminated by chemotherapy. This is associated with an increase in AFP levels in the blood.
- Embryonal carcinoma can raise AFP and HCG levels in the blood. They account for about 40% of testicular cancers. They get their name from the fact that they resemble tissues of early embryos under the microscope. There is a high possibility of metastasis for this type of cancer.
- Choriocarcinoma is fast-growing cancer in adults, but rare. They are high-risk as they can easily spread to the lungs, brain, and bones. It increases blood HCG levels.
- Teratomas are tumours that, under the microscope, look like the three layers of a developing embryo, namely, the endoderm, mesoderm, and ectoderm. They are not associated with tumour cell markers.
Apart from cancers arising from germ cells, the following categories of testicular cancer could also arise:
- Sex-cord stromal tumours are tumours originating from the hormone-producing tissue of testicles, called the stroma. Most such tumours are benign, but if they spread, it is hard to treat them with radiation or chemotherapy.
- Leydig cell tumour arises from Leydig cells, which produce androgens.
- Sertoli cell tumour comes from Sertoli cells, which protect and nourish the germ cells [4]
- Lymphomas are the most common type of secondary testicular cancer, more common in males above 50 years of age.

Diagnosis of Testicular Cancer
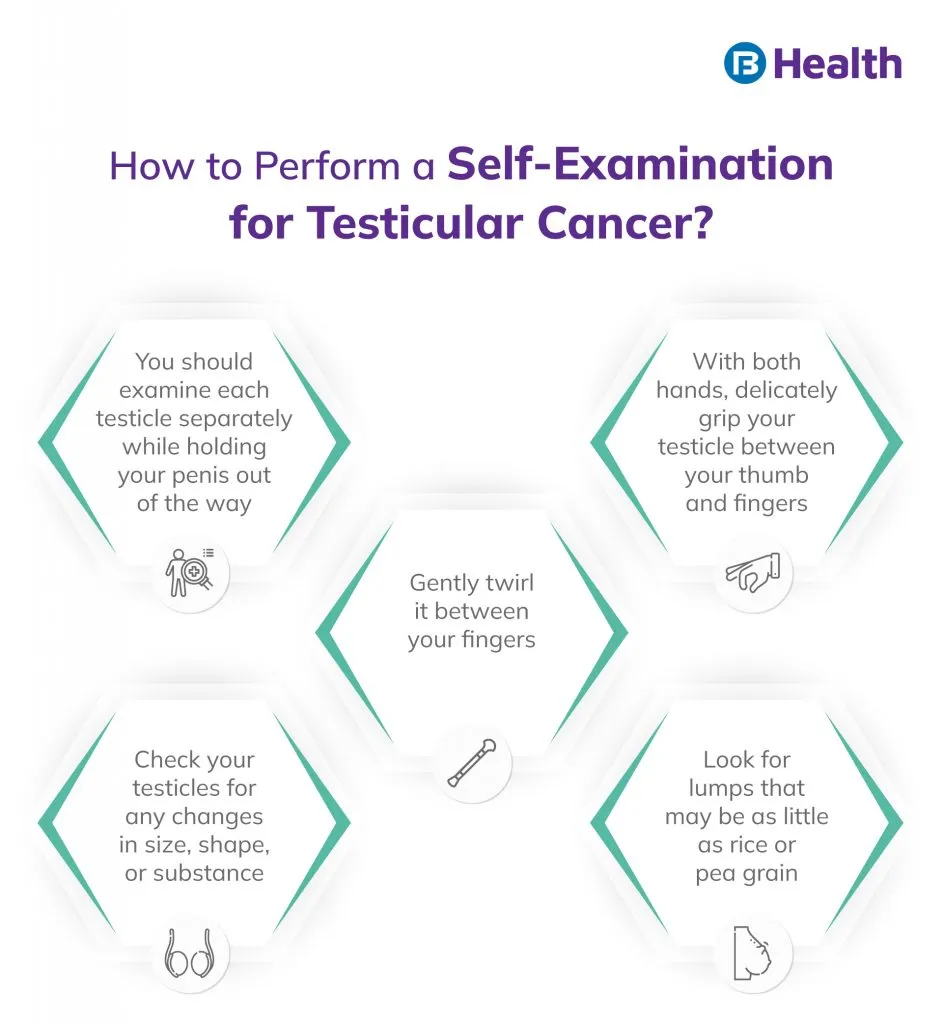
The detection of testicular cancer is fairly easy. It can either be performed by oneself through a self-exam or through a professional medical exam. To elaborate:
Self-exam:
The most suitable time and condition to perform it is when the scrotum is entirely relaxed. It is important to feel the entire surface of the scrotum thoroughly and understand if any region of it feels different from the others. The other anomaly to notice is the presence of any obstruction, such as lumps or bumps within or on the scrotum. If there are any concerns post a self-exam, it is advisable to check in with a doctor.
Medical exam:
The primary form of the check-up is done by a doctor or a cancer specialist, who physically examines the patient to assess his body. Consequently, blood tests to check tumour markers such as alpha-fetoprotein (AFP), beta human chorionic gonadotropin (beta-hCG), and lactate dehydrogenase (LDH) should be conducted to confirm testicular cancer. A testicular ultrasound can also be performed to investigate the interiors of the scrotum and testes. A biopsy may be carried out by obtaining a small amount of the affected tissue.
Additional Read: Prostate Cancer SymptomsTreatment of Testicular Cancer
Treating testicular cancer involves surgical removal of the testes, radiation therapy, and chemotherapy.
Surgery:
A variety of surgical routes can be opted for, depending upon the stage and the extent of the spread of cancer.
- Orchiectomy is the surgical removal of the affected testis along with the tumour mass through an incision in the groin. It also involves closing all blood and lymph vessels arising in this area to stop cancer from metastasizing to parts of the body. It is a key procedure in treating all types of testicular cancer in different stages.
Even after this procedure, the patient can continue living a normal lifestyle as one testicle is sufficient to produce enough testosterone. If desired, a prosthetic testicle can be opted for.
RPLND:
Retroperitoneal lymph node dissection (RPLND) is an intricate surgery involving the removal of lymph nodes from the rear side of the abdomen. It is mostly applicable for men with non-seminomatous germ cell tumours and for those with a high risk of recurrence.
TSS:
Testis-sparing surgery (TSS), as the name suggests, is the removal of only the mass from the testicle, leaving the testicle intact. To allow this, the size of the mass should be very small. This procedure necessitates strict surveillance as the chances of the cancer returning is high.
Radiation:
This form of therapy utilizes X-rays to irradiate and kill cancer cells directly. It is mostly applicable to seminomas since certain non-seminomas are resistant to X-rays. Radiotherapy is utilized to prevent the return of cancer after surgery. A handful of side effects come hand in hand with radiotherapies, such as fatigue, diarrhoea, and skin soreness, but they can be combated with medication.
Chemotherapy:
The use of drugs to treat cancers is termed chemotherapy. The primary mode of administration of the drugs is intravenously, and generally, the position of the vein is kept constant during treatment. This is implemented in case cancer has spread beyond the testicles or if it has recurred after surgery. The mechanism of action of chemotherapy is that drugs, like cisplatin or bleomycin, traverse through the bloodstream and kill cancer cells, but healthy cells also get affected in the process.
This leads to side effects like hair loss, extreme tiredness, infections, and loss of appetite, to name a few. However, there are options to treat the side effects; they generally improve after completing a chemo session.
Additional Read: Thyroid Cancer CausesTesticular Cancer Complications
The most concerning complication that can arise post-treatment of testicular cancer is infertility. There might be a decrease in sperm production and a problem with ejaculation. However, there are drugs to ease those issues. It is also advisable to create a sperm bank prior to treatment so that conceiving is not that difficult in the future. Gradually, the healthy testicle will be primed to produce sufficient testosterone. Ideally, a visit to the doctor once a year or an online doctor consultation to update them about your healing to keep track of the hormones would be recommended. Studies have shown that those who have had testicular cancer have a higher disposition to developing second primary cancers. The most common type of cancer that can emerge after seminomas are thyroid cancer, having the highest probability, followed by cancer of the connective tissue. Prostate cancer also accounted for ¼ of the second primary cancers in a study. Colorectal cancer was shown to arise as a result of non-seminomas [5]
Exposure to radiation and chemotherapy can serve as a risk factor for developing heart disease. It would thus be advisable to maintain a lifestyle that does not contribute to aggravating heart health. For instance, making small changes like eating healthy, incorporating light exercises or yoga or breathing exercises, and eating less sugar can majorly impact a person's health.
Additional Read: What Is Colorectal CancerTesticular Cancer Prevention
There is no steadfast means of preventing testicular cancer. What can be done is to look out for the symptoms and take immediate action if any noticeable change in the normalcy of the testes is observed.
Follow-up is a crucial factor when it comes to any type of cancer. The risk of recurrence of this type of cancer is minor, at most 5% or even lesser. If cancer returns, the earlier a visit to a cancer specialist is scheduled, and the quicker the measures are taken, the better. It is most important to be self-aware and in touch with one's own body so that if there is a possibility of developing testicular cancer, it is caught at the very initial stages and completely eradicated. For any queries or further information, you may contact Bajaj Finserv Health and avail of online doctor consultation. You have the option of arranging an oncologist consultation with our experts. Sign up right away to live a cancer-free life!
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6626920/
- https://erc.bioscientifica.com/view/journals/erc/24/3/119.xml
- https://pubmed.ncbi.nlm.nih.gov/20920735/
- https://www.ncbi.nlm.nih.gov/books/NBK558916/
- https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0214410
Disclaimer
Please note that this article is solely meant for informational purposes and Bajaj Finserv Health Limited (“BFHL”) does not shoulder any responsibility of the views/advice/information expressed/given by the writer/reviewer/originator. This article should not be considered as a substitute for any medical advice, diagnosis or treatment. Always consult with your trusted physician/qualified healthcare professional to evaluate your medical condition. The above article has been reviewed by a qualified doctor and BFHL is not responsible for any damages for any information or services provided by any third party.