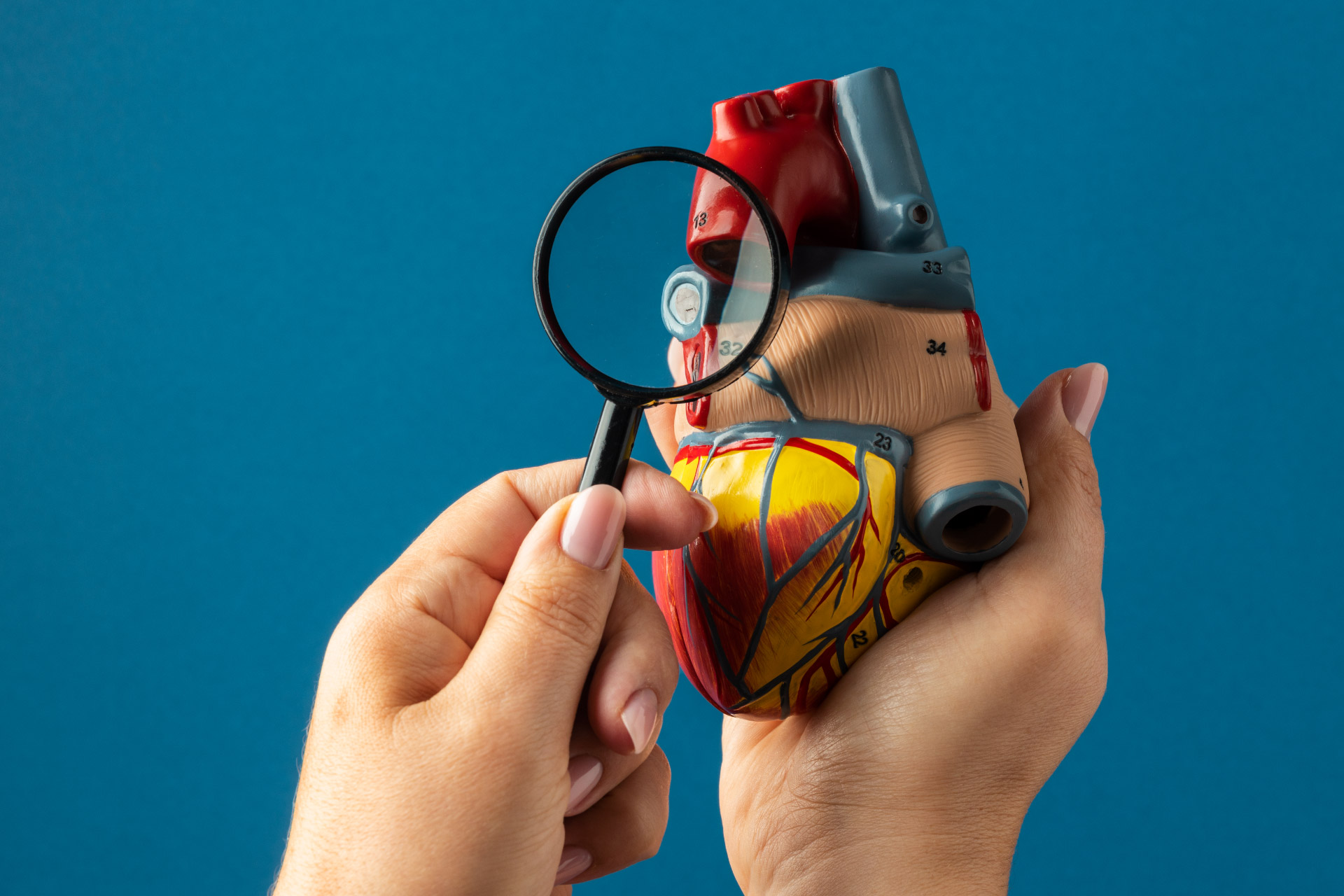
Heart Health | 15 min read
What Are the Causes and Symptoms of a Heart Attack? How to Take Precautions?
Medically reviewed by
Table of Content
Key Takeaways
- Heart disease is among the top causes of death in the world
- Older, overweight, and obese people are more prone to a heart attack
- The risk of a heart attack is lesser when you follow a healthy lifestyle
A heart attack occurs when the blood flow to the heart gets blocked. This results in starving the oxygen supply. It are also termed myocardial infarctions (MI). Getting timely treatment is crucial to surviving such a condition. Without it, a heart attack can lead to cardiac arrest, where the heart stops working completely.
According to the World Health Organization (WHO), 17.9 million people die each year, globally, due to cardiovascular diseases (CVDs). It is among the leading causes of death in both men and women. To know more about the various heart attack causes, symptoms, and tips on how to prevent it, read on.
Things to Know About a Heart Attack
A heart attack happens when the blood flow to the heart is reduced or terminated. Lack of oxygen-rich blood to the heart might cause damage to the affected region. As a result, the heart muscle starts to degenerate.
When your heart isn't getting the blood and oxygen it needs to function properly, you're more likely to get heart failure and other harmful effects.
A heart attack is a severe medical emergency that threatens your life. The sooner you get the treatment you need to get your heart's blood flow back to normal, the better your chances of having a successful surgery.
What Are the Common causes of a Heart Attack?
Blockages in one of the blood arteries that supply blood to your heart cause the great majority of heart attacks. This is most typically caused by plaque, a sticky material that can accumulate on the insides of your arteries (similar to how pouring grease down your kitchen sink can clog your home plumbing). This accumulation is known as atherosclerosis.
Sometimes, plaque deposits within the coronary (heart) arteries might split open or burst, resulting in a blood clot formation where the rupture occurred. If the clot obstructs the artery, the heart muscle may be deprived of blood, resulting in a heart attack.
Heart attacks can also occur without a blockage, but this is uncommon, accounting for around 5% of all heart attacks. This type of heart attack may be caused by a variety of causes, including:
Spasms of the coronary arteries
Uncommon medical problems: Any condition that produces significant constriction of blood arteries is an example of this
Trauma: This includes coronary artery rips or ruptures
Obstruction that originated elsewhere in your body: An embolism is a collection of blood or air bubble that becomes stuck in a blood vessel
An electrolyte imbalance has occurred in the body
Eating disorders can harm your heart over time, leading to a heart attack
Takotsubo, also known as stress cardiomyopathy, can cause heart attacks
Anomalous coronary arteries are congenital cardiac abnormalities in which the coronary arteries are positioned differently in your body than they should be. (The compression of these arteries causes a heart attack)
Blockage in one or more arteries is the most common cause of a heart attack. Plaque, a build-up of cholesterol and other fatty substances, can form in the arteries. This makes them narrower than normal. During a attack, the plaque ruptures, then causes blood clots that block the blood from flowing through the coronary artery. This deprives the heart of oxygen and leads to an attack. Other causes may include low oxygen levels in the blood and misuse of drugs.
Consuming drugs like cocaine and tobacco can cause spasms that prevents the flow of blood to the heart muscles. There are certain risk factors too that can cause a heart attack. These include your age, smoking and drinking habits, high blood pressure, stress, bad cholesterol, obesity, diabetes, and more. Lack of physical activity, metabolic syndrome, and family history with heart attacks can contribute to the list of causes.

Who is More Prone to Heart Attacks?
Several important variables influence the chance of having a heart attack. Unfortunately, you have little control over some of these risk factors for heart attacks.
Based on Age and Gender Factor:
- Men: At age 45, the chance of a heart attack rises significantly
- Women: After menopause or around age 50, the chance of a heart attack rises significantly
Based on Family History of Heart:
Your danger goes up if you are:
- At age 55 or younger, your father or a brother was identified as having heart disease
- At 65 or younger, your mother or a sibling was identified as having heart disease
Based on Life Style:
These factors raise your chance of having a heart attack:
- Absence of exercise
- A diet that is heavy in fat, sugar, and salt
- Using tobacco or smoking
- Overindulging in booze
- Drug abuse (especially in younger people)
Based on Diseases:
These medical disorders can make you more vulnerable to a heart attack:
- Diabetes
- Obesity
- Elevated blood pressure (hypertension)
- High triglycerides (hyperlipidemia)
- Preeclampsia during pregnancy in the past
- Disorders of eating (especially in younger people)
What Are Common Heart Attack Symptoms?
Angina
Angina is not a disease or condition. Instead, it is a symptom that occasionally might indicate a heart attack. The symptoms may be brought on by routine tasks or exercise, but they would disappear after resting or taking nitroglycerin.
You may feel the following symptoms mentioned below:
- In the middle of the chest, there may be pressure, discomfort, squeezing, or a sensation of fullness
- Discomfort or pain in the jaw, neck, back, shoulder, or arm
Suppose you have "stable" angina, which is the most frequent type. In that case, your symptoms will typically occur with known stimuli (such as a strong emotion, physical activity, extreme hot and cold temperatures, or even a heavy meal). The symptoms will go off if you relax or take the nitroglycerin recommended by your doctor.
- Pressure, ache, or tightness in your chest
- Pain in arms that may spread to your neck, throat, jaw, or back
- Heartburn
- Indigestion
- Abdominal pain
- Nausea
- Breathlessness
- Sweating
- Vomiting
- Sudden dizziness
- Fatigue
Additional Read: Best Exercises to Strengthen Your Heart
Pre-Heart Attack Symptoms in Females:
Symptoms might vary from person to person or from one heart attack to the next. Women are more prone to have the following heart attack symptoms:
- Unusual exhaustion
- Breathing difficulty
- Nauseousness or vomiting
- Feeling dizzy or lightheaded
- Discomfort in your stomach. It might be indigestion.
Neck, shoulder, or upper back discomfort
Pre Heart-Attack Symptoms Male:
The study does warn, however, that males are more likely to report fewer common symptoms, including heartburn, back discomfort, or indigestion-like pain.
Most Common Symptoms
Pain in the chest. Most heart attacks are characterized by discomfort in the centre of the chest that lasts more than a few minutes, or that arises, departs, and then reappears. In addition, painful pressure, squeezing, fullness, or uneasy pressure may be experienced.
Discomfort in various upper body regions. Some symptoms include back, neck, jaw, or stomach pain, discomfort, and pain in one or both limbs.
Breathing difficulties, either with or without chest pain.
How to Prevent Heart Attack?
You can prevent a heart attack by making healthier lifestyle choices. Some of these are as follows.
Quit smoking
Smoking is injurious to you and those around you as raises the risk of heart disease. So, quit smoking for a healthy heart.
Eat healthy
Eat heart healthy foods. Fill your diet with fruits and vegetables. Consume food items that are rich in Omega 3 fatty acids such as fish, avocado, and olive oil.
Maintain a healthy body weight
People who are obese or overweight are at a higher risk of cardiovascular disease. [4] Speak to a doctor about your ideal body weight and take active steps towards maintaining it. By doing so, you can improve your cholesterol levels as well as heart health.

Exercise
Doing physical exercise on a regular basis reduces the risk of a heart attack. It also lowers your blood pressure and bad cholesterol, while increasing good cholesterol. Exercising for 30 minutes a day is enough to see results. Cardiovascular exercises like swimming or brisk walking are a great help. For even better results, try guided strength or weight training as well.
Limit alcohol
Drinking alcohol increases your blood pressure and heart rate. It also makes you gain weight by increasing fat levels in your blood. So, avoid drinking alcohol completely or consume it in moderation.
Avoid stress
Stress leads to anxiety, which is harmful. Talk to your family and friends or sign up for a stress management program. Physical exercise and meditation can also help.
Additional Read: How to Prevent Heart Attack?How can you Manage Heart Attacks?
The injured cardiac muscle must get blood flow as quickly as feasible to treat a heart attack. There are many different methods for this that range from taking drugs to surgery. However, it's quite likely that the therapy will use several of the following techniques.
More oxygen supplies
Supplemental oxygen is frequently given along with other heart attack therapies to people experiencing difficulty breathing or having low blood oxygen levels. To breathe the oxygen, you can use an artificial tube that sits just below your nose or a mask that covers your nose and mouth. This eases the pressure on your heart and increases the quantity of oxygen flowing in circulation.
Grafting a coronary artery
Coronary artery bypass grafting may be used to treat people with significant coronary artery blockages. Open-heart surgery, bypass surgery, or CABG (in case you are wondering, the abbreviation is pronounced "cabbage") are common names for this procedure.
In CABG, a blood artery from another part of your body is used to create a blood detour, often from your chest, arm, or leg. This provides blood to your cardiac muscle and redirects blood to one or more obstructed artery parts.
Invasive coronary procedures
A method known as percutaneous coronary intervention (PCI) is used by providers to reestablish blood flow to your injured heart muscle. This involves inserting a catheter-based device into a large blood vessel (usually one near your upper thigh or your wrist).
The sooner blood flow is restored with the help of PCI, the better the chances of a successful outcome. Hospitals gauge their capacity to treat a heart attack using a statistic known as "door-to-balloon time." This is the typical amount of time it takes for patients to receive PCI following their initial visit to the emergency room. In order to keep the artery open and prevent further blockages in the same location, PCI frequently entails the implantation of a stent at the site of the obstruction.
Medications
- Nitroglycerin: This medication eases chest discomfort and widens blood arteries to allow for easier blood flow
- Anti-arrhythmia drugs: Heart attacks frequently result in arrhythmias, abnormalities in your heart's regular beating rhythm that can be fatal. These malfunctions can be stopped or avoided using anti-arrhythmia drugs
- Painkillers: Morphine is the most frequently prescribed painkiller for heart attack treatment. Chest pain can be lessened by doing this
- Providers only utilize thrombolytic (clot-busting) drugs within the first 12 hours following a heart attack
- Aspirin and other blood-thinning treatments are within the category of anti-clotting drugs
Is it Possible to Reduce the Risk of Having a Heart Attack?
There are numerous ways you can take care of yourself and lower your chance of having a heart attack, even if there are certain risk factors that you can't change. The steps you can take consist of the following:
Frequent checkups: Find a primary care physician and schedule a checkup or wellness appointment at least once yearly. Many early warning symptoms of heart disease, including those you can't feel, can be found at an annual exam. Your heart rate, blood pressure, blood sugar, cholesterol, and other measurements are included in this group.
Stop using tobacco products: This applies to all e-cigarettes and tobacco products that are available in the market.
Regular exercise: Aim for 30 minutes of moderately vigorous exercise five days a week.
Consume a nutritious diet: Examples include the Dash or Mediterranean diets. A plant-based diet is a fantastic substitute that can give you good health.
Keep your weight at a healthy level: Your primary care physician can suggest a healthy weight for you and offer you tools and suggestions to help you get there.
Maintaining your current health: Diabetes, high blood pressure, and excessive cholesterol are diseases that need to be taken care of on a daily basis.
Become less stressed: Think about yoga, deep breathing, and meditation exercises to reduce stress levels.
Medications: Don't merely take drugs when you remember to or when you have a doctor's visit coming up; instead, take them as directed.
Keep up with your medical appointments: Regular visits to your doctor might help you find heart problems or other health conditions you weren't aware of. This can help resolve problems quickly.
You may actively support your health without entirely changing your way of living. Consult your primary care physician and other medical personnel for advice. They can offer you the resources and information you require.
Your doctor will advise a cardiac rehabilitation program if you've already experienced a heart attack. The purpose of this program is to lessen your risk of having another heart attack. The same healthy living objectives outlined above are the emphasis of these medically supervised programs, which also provide counselling.
What are the Complications of a Heart Attack?
A heart attack may lead to several consequences. First, a heart attack can alter your heart's rhythm and cause it to stop entirely. Arrhythmias are the name for these irregular rhythms.
Some cardiac tissue may perish if your heart's blood supply is cut off during a heart attack. As a result, your heart may weaken, leading to serious issues, including heart failure.
Your heart valves may be damaged by heart attacks and develop leaks.
Heart attack can also put your body in cardiogenic shock. You may feel symptoms such as difficulty in breathing, pale skin, chills in body, and mental confusion.
How quickly you obtain medical attention and how much of your heart has been damaged by the heart attack will influence the long-term repercussions on your heart.
Some uncommon complications of heart attack:
Cardiovascular shock: This uncommon ailment happens when the heart's ability to pump blood is suddenly and unexpectedly lost.
Inflammation of the heart's pericardial sac-like tissue (pericarditis): Sometimes, a heart attack sets up an unfavourable immunological response which is called Dressler syndrome/ post-myocardial infarction syndrome/post-cardiac damage syndrome.
Coronary arrest: In this case, the heart stops abruptly. Sudden cardiac arrest is brought on by an abrupt change in the heart's signals. This illness seriously threatens life, and heart attacks enhance the risk. Without prompt treatment, it may result in death (sudden cardiac death).
Heart bleeds: Heart ruptures, in which the heart's muscles, walls, or valves separate, are extremely dangerous but relatively uncommon complications of a heart attack (rupture). It often occurs 1 to 5 days after a heart attack and can occur if the heart sustains considerable damage.
Processes to Go Through If you Have This Condition
You have an increased chance of experiencing another heart attack after one. Therefore, your healthcare professional will likely advise additional monitoring, testing, and treatment to prevent further heart attacks. A few of these are:
Heart scans
These can evaluate the impact of your heart attack and identify whether you have permanent heart damage. They are similar to the techniques used to diagnose a heart attack. In addition, they might search for indications of circulation and cardiac issues that raise the risk of future heart attacks.
Stress test
While exercising, your heart will undergo a series of tests and scans that might detect any issues that would otherwise go undetected.
Physical activity
Discuss your daily activities at work and in your personal life with your healthcare staff. After a heart attack, your doctor could advise you to take a break from work, travel, or sexual activity.
Cardiac rehabilitation
These courses assist you in enhancing your general well-being and way of life, which can help you avoid having another heart attack.
You'll also keep taking medications over time, including some of the ones you were given for acute heart attack therapy. These consist of the following:
- Beta-blockers
- ACE blockers
- Medications that cause thinning of the blood, such as aspirin
Lifestyle adjustments: Along with taking prescription medications, making lifestyle changes like following a healthier diet, getting more exercise, saying no to smoking, and managing stress can help you live a healthier life. To incorporate these lifestyle changes, inquire about participating in a cardiac rehabilitation program with your medical team.
A few more processes include
- Taking measures to maintain a healthy range for your blood pressure and cholesterol
- Avoiding physical exertion, especially right after a heart attack
- Consuming a nutrient-dense, balanced diet low in saturated and trans fats, depending on what your doctor approves, and engaging in light to moderate activity
- Reducing weight if you are overweight
- Giving up smoking
- Monitor your blood sugar levels regularly if you have diabetes
Medication and treatment
Follow your doctor's advice and prescription. If you have heart disease, you can avoid an attack with proper medication. If you haven’t been diagnosed, your doctor may conduct tests like x-rays, CT scans, echocardiograms, electrocardiography, blood tests, and cardiac catheterization.
Based on these, treatments include balloon angioplasty, stent placement, and bypass surgery. Some drugs that are given during heart attack include aspirin, antiplatelet drugs, and thrombolytic therapy.
Additional Read: Heart Healthy Diet: 15 Foods You Should EatDiagnosis of a Heart Attack: Steps and Processes
Medical professionals in an emergency department scenario often diagnose heart attacks. Anyone exhibiting heart attack symptoms should have a physical examination, including listening to the heart and lungs and measuring blood pressure, oxygen levels in the blood, and pulse.
A medical professional will use the following to identify a heart attack:
- History of Medical Records: Your medical professional will inquire about your medical history and symptoms. They could also request a description from a companion who was present.
- Blood tests: The destruction of heart muscle cells during a heart attack nearly invariably results in the appearance of a chemical marker, a cardiac troponin, in your circulation. One of the most accurate ways to identify a heart attack is through blood tests that search for that signal.
- Electrocardiogram (EKG or ECG): When you visit an ER with heart attack symptoms, one of the first tests you receive is an electrocardiogram (EKG or ECG).
- Echocardiogram: An echocardiogram creates an image of your heart's inside and exterior using ultrasound (high-frequency sound waves).
- Angiogram: An angiogram reveals regions with little or no blood flow.
- CT Scan: Using computed tomography (CT), your heart is thoroughly scanned.
- MRI Scan: A strong magnetic field and computer processing are used in the cardiac MRI exam to produce a picture of your heart.
- Nuclear heart scans: These scans, like angiography, involve injecting a radioactive dye into your blood. They employ computer-enhanced techniques, such as computed tomography (CT) or positron emission tomography (PET) scans, distinguishing them from angiography.
As soon as you notice any heart attack symptoms, consult a doctor immediately. If you are alone and suspect the onset of a heart attack, call for medical emergency services. Chew an aspirin until they arrive and do not drive to a medical center. These are emergency protocols to follow and can be avoided altogether with the right care. For proper preventive and reactive care for heart disease, book an appointment with the top doctors using the Bajaj Finserv Health platform.
References
- https://www.heart.org/en/health-topics/cardiac-arrest/about-cardiac-arrest
- https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1
- https://www.cdc.gov/heartdisease/facts.htm
- https://my.clevelandclinic.org/health/articles/17308-obesity--heart-disease
Disclaimer
Please note that this article is solely meant for informational purposes and Bajaj Finserv Health Limited (“BFHL”) does not shoulder any responsibility of the views/advice/information expressed/given by the writer/reviewer/originator. This article should not be considered as a substitute for any medical advice, diagnosis or treatment. Always consult with your trusted physician/qualified healthcare professional to evaluate your medical condition. The above article has been reviewed by a qualified doctor and BFHL is not responsible for any damages for any information or services provided by any third party.