Orthopaedic | 7 min read
What is Osteomyelitis: Causes, Symptoms, Treatment
Medically reviewed by
Table of Content
Synopsis
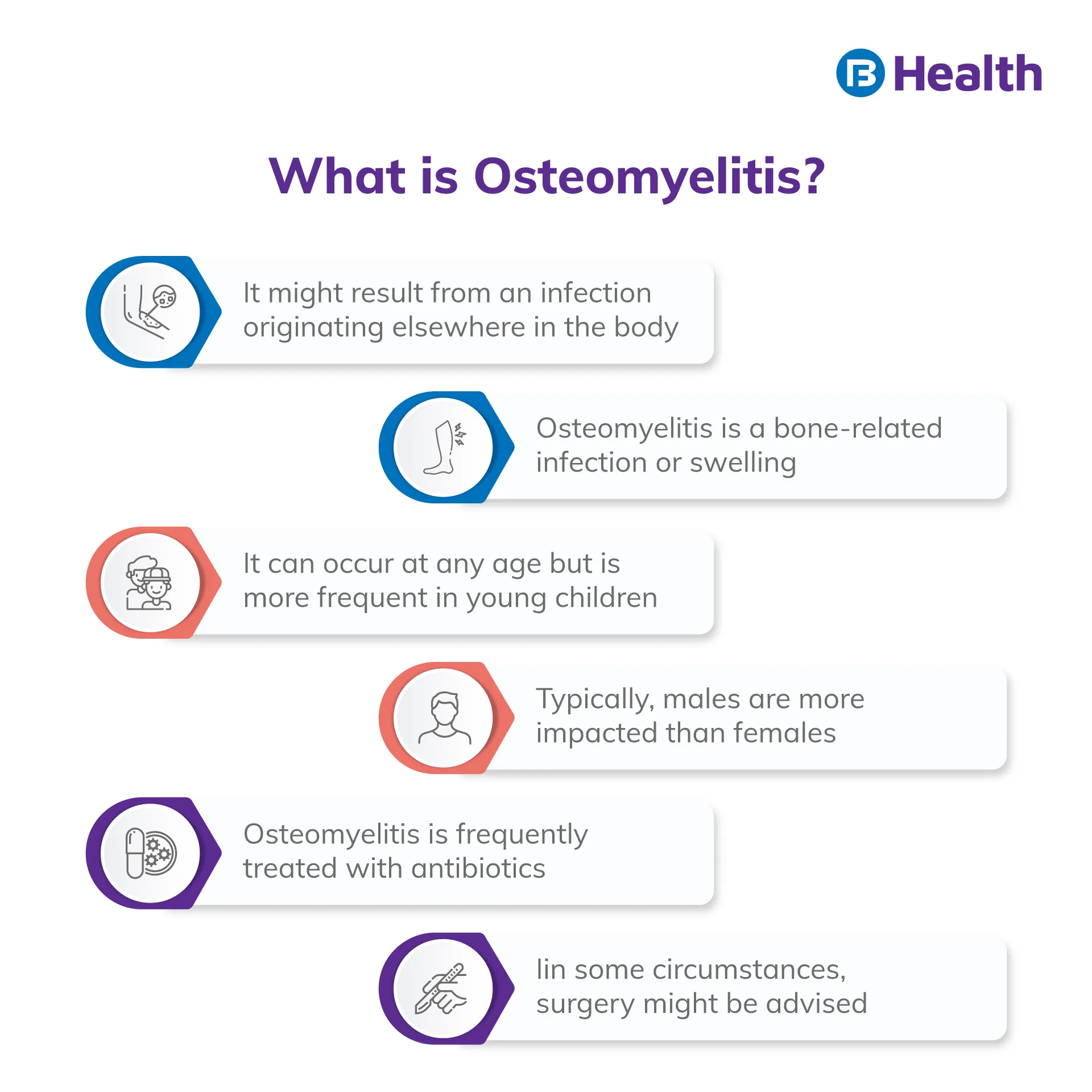
Osteomyelitis is an inflammation or swelling of bone tissue, usually resulting from an infection. The typical infectious agents here are bacteria. The two most common entry pathways are through a primary bloodstream infection and a wound or injury that allows germs to enter the bone.
Key Takeaways
- The blood flow may propagate an infection from other parts of the body to the bones
- The direct invasion via surgery, open fractures, or objects that pierce the bone
- Infections in adjacent structures, such as soft tissues or joints, are natural or artificial
Causes Osteomyelitis
Spread through the blood
Infection often happens in the bones when organisms that cause osteomyelitis break out via circulation. It typically happens in:
- The ends of arms and leg bones of children
- Adults' spines, especially those of older persons
Vertebral osteomyelitis is the term used to describe infections of the vertebrae. Vertebral osteomyelitis is more common in those who are elderly or disabled such as those living in nursing homes, have sickle cell disease, get renal dialysis, or inject medicines using non-sterile needles.
Staphylococcus aureus is the bacterium that most frequently causes osteomyelitis and travels via the bloodstream. Mycobacterium tuberculosis, the bacteria that causes tuberculosis, and fungi can spread similarly and result in osteomyelitis. It can especially happen to people with weakened immune systems (like those with HIV infection, certain cancers, or who are receiving treatment with immunosuppressive drugs) or who live in areas where specific fungi infections are prevalent.
Direct invasion
Through open fractures, during bone surgery, or through contaminated things that enter the bone, bacteria or fungus seeds, sometimes known as spores, may directly infect the bone. For example, osteomyelitis may develop when a metal implant has been surgically inserted into a bone to treat a hip fracture or another type of fracture. Additionally, the bone to which an artificial joint (prosthesis) is connected may get infected with bacteria or fungus spores. Then, during a joint replacement procedure, organisms may be transferred into the region of bone around the prosthetic joint, or the infection may develop later.
Spread from surrounding structures
Another factor that might cause osteomyelitis is a neighboring soft tissue infection. After a few days or weeks, the infection spreads to the bone. Older folks are more prone than younger people to the spread. Such an infection may begin in a location that has been harmed by radiation therapy, cancer, surgery, or an injury. Or it may begin in a skin ulcer—particularly on the foot—caused by inadequate blood flow or diabetes. In addition, the skull may get infected with a sinus, gum, or tooth infection.
Who Gets Osteomyelitis
It is rare and affects two people out of 10,000. Although in diverse ways, the illness impacts both children and adults. The chance of developing osteomyelitis is increased by many immune-compromising ailments and practices, such as:
- Diabetes (most cases of osteomyelitis stem from diabetes)
- Acute myeloid leukemia
- AIDS or HIV
- Rheumatoid Arthritis
- Usage of intravenous drugs
- Alcoholism
- Long-term steroid usage
- Hemodialysis
- Low blood flow
- Recent harm
- Surgery on the bones, such as hip and knee replacements, raises the risk of bone infection.
Osteomyelitis in Children and Adults
Osteomyelitis in children is often acute. Compared to chronic osteomyelitis, acute osteomyelitis develops more quickly, is simpler to treat, and has a better prognosis. It typically manifests in the arm or leg bones of kids. Osteomyelitis in adults can be either acute or persistent. Chronic osteomyelitis, which continues or recurs after therapy, is more common in those with diabetes, HIV, or peripheral vascular disease. Osteomyelitis frequently affects an adult's pelvic or spine vertebrae, whether it is acute or chronic. Additionally, it can happen in the foot, especially if a person has diabetes.

Symptoms of Osteomyelitis
There are several Osteomyelitis symptoms. Infections of the leg and arm bones can result in fever and, occasionally, discomfort in the infected bone for days after acute osteomyelitis spreads through the blood. The movement might be uncomfortable, and the region above the bone could be sore, red, heated, and swollen. The person could feel exhausted and lose weight. In the tissue nearby, abscesses might develop.
Pain in the vicinity of an infected prosthetic joint or limb is frequently chronic. Vertebral osteomyelitis typically takes time to manifest, resulting in chronic back discomfort and touch sensitivity. Movement worsens the discomfort, and resting, applying heat, or using painkillers don't help (analgesics). Fever, which is typically the most evident indication of an infection, is frequently absent.
If osteomyelitis is not properly treated, chronic osteomyelitis may occur. It is a chronic infection that is exceedingly challenging to cure. As a result, chronic osteomyelitis can occasionally go unnoticed for months or even years without showing any signs. The more typical symptoms of chronic osteomyelitis include persistent infections in the soft tissue surrounding the bone, bone pain, and intermittent or continuous pus leakage through the skin. A sinus tract grows from the diseased bone to the skin's surface, and pus drains down the sinus tract to cause this discharge.
How is Osteomyelitis Diagnosed?
- A blood test
- X-rays, computed tomography (CT)
- Magnetic resonance imaging (MRI)
- A bone scan is an example of an imaging procedure
Osteomyelitis may be suspected by symptoms and abnormalities discovered by doctors during a physical examination. For instance, physicians could think someone has osteomyelitis if they have chronic, inexplicable pain in a bone, etc.
Occasionally, it takes 2 to 4 weeks following the onset of symptoms for an x-ray to reveal abnormalities typical of osteomyelitis. Computed tomography (CT) or magnetic resonance imaging (MRI) is performed if the results of the x-ray are uncertain or if the symptoms are severe. For identifying osteomyelitis, MRI offers the greatest combined sensitivity and specificity (78% to 90% and 60% to 90%, respectively). Within 3 to 5 days of the start of the illness, it can spot an early bone infection.[1] The diseased joints or places can be located using CT or MRI, showing any adjacent illnesses like abscesses.
An alternative procedure is a bone scan, which involves injecting radioactive technetium and creating pictures of the bone. Except for babies, when scans may not consistently detect abnormalities in developing bones, the diseased region always appears abnormal on bone scans. However, a bone scan often cannot detect infections due to other bone conditions.
Additional Read: Rickets diseaseOsteomyelitis Treatment
Osteomyelitis treatment comprises the following:
- Antifungal medications or antibiotics
- Occasionally, surgery
- Usually, drainage is used for abscesses
Antifungal and antibiotic medications
Antibiotics are the most effective treatment for children and adults who have recently contracted bone infections through the bloodstream. Broad-spectrum antibiotics, effective against Staphylococcus aureus and many other types of bacteria, are administered if the bacterium causing the illness cannot be identified. Antibiotics may be administered intravenously for 4 to 8 weeks, depending on the severity of the illness.
Depending on how the patient reacts, oral antibiotics may then be continued. Some patients require months of antibiotic therapy because they have persistent osteomyelitis. In addition, antifungal medications are necessary for several months if a fungal infection is found or suspected. However, surgery is typically not required if the infection is detected early on.
Operation and drainage
The typical course of treatment for individuals with bacterial osteomyelitis of the vertebrae is antibiotics for 4 to 8 weeks. Sometimes the patient has to stay in bed and may need to wear a brace. Surgery may be required to empty abscesses or stabilize damaged vertebrae (to prevent the vertebrae from collapsing, thereby damaging nearby nerves, the spinal cord, or blood vessels). Treatment is more difficult when a neighboring soft tissue infection brings on osteomyelitis.
The dead tissue and bone are often surgically removed, and the empty region is then filled with good skin or other tissue. Antibiotics are then used to treat the infection. After surgery, broad-spectrum antibiotics may be needed for more than three weeks. Typically, an abscess has to be surgically emptied when it is present. Surgery can also be necessary for those who have prolonged fever and lose weight.
For more information and help, contact Bajaj Finserv Health to speak to an osteopath. You can schedule an online consultation from your home to receive the right advice regarding osteomyelitis and live a pain-free, healthy life.
References
- https://pubmed.ncbi.nlm.nih.gov/22046943/
Disclaimer
Please note that this article is solely meant for informational purposes and Bajaj Finserv Health Limited (“BFHL”) does not shoulder any responsibility of the views/advice/information expressed/given by the writer/reviewer/originator. This article should not be considered as a substitute for any medical advice, diagnosis or treatment. Always consult with your trusted physician/qualified healthcare professional to evaluate your medical condition. The above article has been reviewed by a qualified doctor and BFHL is not responsible for any damages for any information or services provided by any third party.